There’s no question telehealth is here to stay. After all, why would anyone want to go to the doctor’s office when a video call will suffice? Telehealth is far too convenient to vanish for good—but don’t get too comfortable. If you don’t take the time to prepare your telehealth practice for a reopened economy, you may vanish in a sea of other outdated practices.
Once the COVID-19 pandemic ends, the healthcare market will ripe for the taking. Only a few practices will emerge unscathed and ready to serve. Where will you stand?
How Telehealth Started Booming
Telehealth is booming. By mid-April, urgent telemedicine visits more than doubled, and non-urgent visits grew more than 4000%. As a result, telehealth startups like Medici have secured massive rounds of funding. It’s easy to see why: many checkups, such as medicine checks, don’t require a patient to be in office. Moving them online reduces strain on both patients and doctors, and it greatly reduces the risk of infection. This video from the US Department of Health and Human Services beautifully outlines the benefits of telehealth.
These benefits and more make telehealth a wonderful innovation (which you can read more about in our post about healthcare technology), and it’s certainly here for good. Even if just 10% of appointments remain online, Telehealth will have a massive impact on modern healthcare.
But this boom isn’t permanent. Everyone wants this pandemic to end as soon as possible, and once it ends, regulations will tighten, the economy will return to normal, and patients will decide if they prefer online or in-person appointments. What you do during the boom determines if your practice will survive afterward. To keep yourself afloat, we recommend the following three strategies:
Check the Regulations
Thanks to new government regulations, telehealth is simple–for now
The most notable new regulation came at the end of March when the Department of Health and Human Services announced an enforcement discretion for telehealth. Normally, certain communication tools (such as standard phone or video calling software) aren’t fully compliant with HIPPA. However, this enforcement discretion allows doctors to connect with patients using popular private software, such as Facebook Messenger, Google Hangouts, and Skype. This policy was incredibly important since it significantly slowed the spread of COVID-19 and kept both doctors and patients safe, and it still excludes public-facing communication, such as Facebook Live and the ever-growing TikTok.
But it doesn’t stop with HIPPA. Many practices will have noticed that Medicare now extends to several different types of practitioners. The Center for Medicare and Medicaid Services included the following in their press release at the end of April:
For the duration of the COVID-19 emergency, CMS is waiving limitations on the types of clinical practitioners that can furnish Medicare telehealth services. Prior to this change, only doctors, nurse practitioners, physician assistants, and certain others could deliver telehealth services. Now, other practitioners are able to provide telehealth services, including physical therapists, occupational therapists, and speech language pathologists.
The big change here is that therapeutic services may use Medicare for telehealth, too. However, this change is temporary. It will only last as long as the United States remains in a state of national emergency.
So, we have telehealth-friendly regulations. What’s the problem?
Telehealth is certainly going to stick around, and the government will probably pass more telehealth-friendly bills after seeing its success during this crisis. In fact, the government has heavily endorsed telehealth throughout this crisis and into the future.
Even though pro-telehealth bills will almost certainly be passed after this crisis, it’s unwise to assume that the government will translate the current, more extreme emergency policies into concrete, permanent law. These policies are temporary. They were designed to be temporary. If you plan to hold all future non-urgent appointments over Google Hangouts, your practice will suffer.
Here’s our advice: the rules may be lax now, but begin the transition toward stronger HIPPA compliance. Patient data is extremely sensitive, and there’s no problem with being too safe. This means end-to-end encryption is key, which rules out a lot of video chat software. Even Zoom, which is listed by name in the HHS document as “acceptable” telehealth software, is riddled with unacceptable security issues. For your telehealth infrastructure to last long-term, build it to last now.
Long-term telehealth planning is especially important for therapeutic practitioners accepting medicare remotely under the CMS rule changes. These regulations are strictly temporary, so if you rely on digital Medicare patients now, you will struggle when the state of emergency ends.
Overall, prepare for stricter telehealth regulations now. Once the temporary rules change, you’ll be ahead of the game. Even if the government passes permanent telehealth-friendly laws, your practice will be ahead of the game with better, safer technology.
Try Hybrid
Don’t focus solely on optimizing your telehealth practice. Instead, work out ways to integrate online and in-person appointments. In other words, go hybrid.
Instead of working office-first, hybrid practices prioritize online appointments–even for first-time patients. This model wasn’t popular before the pandemic. Even new, tech-savvy practices like Circle Medical would mostly use digital communication for follow-up appointments. However, shelter-in-place measures have forced these practices to pivot, and after building the digital infrastructure to handle online appointments, their productivity has skyrocketed. In fact, Circle Medical secured a seven-figure funding deal after its major pivot toward a telehealth-first model.
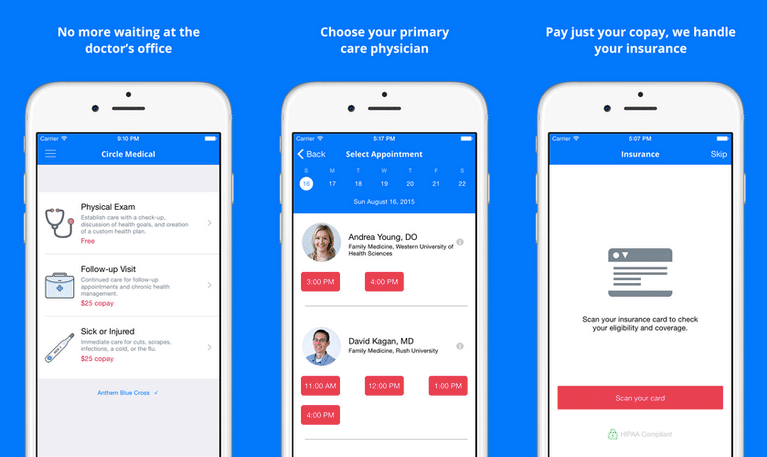
Circle Medical’s new telehealth app (image from Techcrunch)
And who can blame them? A hybrid model empowers practices to cut back on in-office resources, free up extra time, and ease stress for both doctors and patients. Previously, it was much less feasible. But now that patients have had a taste of the convenience of telehealth, hybrid practices are the hyper-efficient model of the future for minimizing expenses and maximizing revenue. Whether you plan to use a pre-existing app or develop your own, consider a hybrid practice to make it even more effective.
Telehealth may be growing now, but hybrid practices are the future. Seriously, give it a shot.
Stay Flexible
Let’s get one thing straight: no plan will be perfect. The situation is changing far too fast to plan perfectly, so your best bet is a flexible framework, not a rigid one.
The COVID-19 outbreak may seem to be drawing to a close, but this is only the beginning, and no one knows what to expect. Anthony Fauci, the director of the National Institute of Allergy and Infectious Disease, says that a second wave is “inevitable.” Other reputable sources are even more pessimistic. A paper published in the American Association for the Advancement of Science predicts that some form of “intermittent social distancing” may last well into 2022.
No one knows for sure how long this crisis will last, but most people agree that there will be three distinct phases
Phase I for Telehealth: Telehealth Boom
We’ve been in Phase I for a while now. Your practice is probably performing excellently since people are staying at home, and most of your appointments are probably conducted with a video chat or over the phone.
However, this phase of booming business is coming to a close. States are slowly reopening and people are trickling out of their homes. Of course, telehealth will remain important, but many patients will transition back into in-office appointments. We may still be in Phase I, but prepare for Phase II
Remember not to leave Phase I too hastily. According to recent estimations, some states still haven’t hit their peak, while others passed their peak in early April. Depending on your state, you may be in this first phase, or you may be transitioning into Phase II. Figuring out which phase your state is in requires some research. Georgia may have been relaxing rules since April 24, but because it reopened so quickly, it likely won’t have a safe reopening until the end of June. Just because your state is opening does not mean you are out of Phase I. Examine the data and do your research before moving to Phase II.
Phase II for Telehealth Apps: Reopening the Marketplace
Phase II (reopening the marketplace) is not the same thing as Phase III (going back to normal). It just means that businesses will be reopening and people will be returning to work. Social distancing may still remain in place, patients may still remain at home, and things may still feel eerily quarantine-esque. However, as it progresses, we will eventually reach Phase III, as the majority of people return to
Phase III for Telehealth Apps: Going Back to Normal
Remember that Phase III doesn’t mean everything will go back to normal; it just means that restrictions will be lifted. The economy will still take a massive blow. Economists predict that we are heading into the worst recession since the Great Depression, and not every company can come out of this crisis unscathed. The economy won’t be the same; it will be irreparably changed, and the most important thing any business can do to survive is to adapt to the changing markets.
Although no one knows for sure what will happen, experts agree on one thing: this pandemic will last for a long time, but not forever. Make sure you keep up with the news and adapt to any possible situation.
What’s Next for Your Healthcare Practice?
Even as the pandemic draws closer to its conclusion, these times are uncertain. In some way or another, everyone has been impacted by this crisis. Even hospitals and healthcare practices are struggling with revenue. To prepare your own practice for whatever this crisis throws your way, consider starting a flexible plan for the future. Don’t forget to keep your eye on the changing regulations, and start striving toward a hybrid model. We know Telehealth is the future of healthcare, but that path is muddy and uncertain. Leave room to adapt and seize every opportunity you can.